6 Latest IVF Techniques That You Should Know About
IVF Clinics, IVF Treatment
Did you know that the success rates for IVF is just 35%? That’s why it’s necessary for you to know about the latest IVF technologies, that can increase the chances of your IVF success. Contrary to what many couples believe, it is perfectly natural to go in for multiple attempts before finally being able to conceive. There has been tremendous advancement in the field of IVF technologies which help couples increase success rates and are used in times of repeated IVF failures. So, to bring you all the nitty-gritty details of latest IVF technologies, Fertility Dost got in a conversation with Dr. Hrishikesh Pai (M.D, F.R.C.OG (UK), F.C.P.S, F.I.C.O.G, M.Sc (USA)) to compile this article. As you scroll down you’ll get to know about the latest options that you can explore, as per your needs.
It’s best for patients to go through a pure IVF cycle without any add-ons for the first two times. If that doesn’t work then you can look for other options.
The Future of IVF: 6 Innovations Improving Pregnancy Chances
For those women who have undergone repeated IVF cycles but are unable to conceive, the first step is to investigate these couples by doing all the blood tests like hormone levels, thyroid and prolactin levels etc. After this there are a number of new technologies which can be used as per the need of the patient. Here’s a list of 6 relatively new techniques which you should know about if you’re trying to conceive. But remember every individual’s situation is different and trusting your doctor is extremely important.
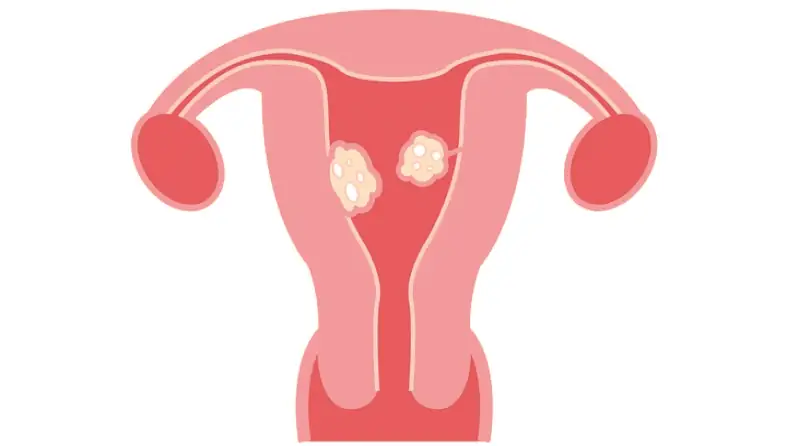
Fertility Enhancing Surgeries
There are several ways to enhance fertility depending on the condition of the patient.
- If there is a fibroid in the uterus, a laparoscope is used to remove the fibroid. If there is adenomyosis in the patient, it’s best to freeze the embryos and then give them Goserelin injection to suppress the adenomyosis for 2-3 months. After this the embryo transfer can be done.
- Some patients have the issue of hydrosalpinx, i.e. water in the fallopian tube due to infection which can get discharged in the uterine cavity and reduce the result. In such cases, the hydrosalpinx should be clipped and blocked so that the water doesn’t get discharged into the uterine cavity.
- If there is an endometrioma which is very large and may come in the way of egg pickup procedure, a laparoscope is used to decompress the endometrioma. There is no need to remove it because if we remove the endometrioma, the patient’s ovarian reserve will reduce.
These are all done pre-operative. Because if there is a poor ovarian reserve or any other issue which can be resolved then it should be treated before starting the IVF cycle.
Preimplantation Genetic Screening (PGS) Technique
Embryos with genetic disorders can lead to IVF failures and miscarriages. PGS Technique is a modern IVF technology solution to this. If you have had multiple IVF failures, opting for PGS is the best option. You will be stimulated to collect a lot of eggs for PGS. Once the embryos are formed, PGS (pre-genetic screening) can be conducted to test the embryos and see if there are any genetic disorders, and the embryos can be frozen. A frozen embryo transfer gives upto 20% better pregnancy rate than a fresh embryo transfer.
State-of-the-art Technology to Improve Results

There are various state-of-the-art technologies that can be used for better success rates.
- A double transfer of embryos can be done i.e, on Day 3 one embryo and on Day 5 one/two embryos (Day 5 blastocyst) are transferred. This method is used to create a higher chance of pregnancy in couples.
- These days for many patients, a new incubator is being used, called the Embryoscope. In this process culturing of the embryos is done and in every 15 minutes photographs of the embryos are taken. Using this method along with genetic analysis we can look at the development of the embryos and predict which of them have the best quality. Using these embryos will give better results in patients with poor ovarian reserve.
- Approximately 10% of patients have incomplete endometrial development. Normally, a woman needs 7-9 mm thickness of the endometrium in order to achieve a good pregnancy rate. So if the endometrium is thinner than 7mm and embryo transfer is done, then it’s not going to work out well. So, in patients with poor endometrium, inserting various chemicals like G CSF (granulocyte-colony stimulating factor) intrauterine, PRP (platelet rich plasma) intrauterine etc. can help to make the endometrial lining better, resulting in improved pregnancy rates following IVF.
If the IVF cycles are still not successful, the couple can consider the option of egg donation.
Laser hatching
Laser Hatching or Assisted Laser Hatching was introduced in India by Bloom IVF in 1998. It is used to improve pregnancy rate in patients. Prior to transferring the embryos, hatching of the embryos is done i.e, it is cut with a laser beam. This technique enables an embryo to attach onto the uterine wall post embryo transfer with increased success rates. This procedure uses a highly specialized and focused infrared laser beam to remove very carefully the outer protective cover of the embryo or the “Zona Pellucida” which allows for easier uterus implantation.
This technique has proven to considerably improve the success rates of women trying to conceive via IVF. In general, this technique is specifically performed for women above the age of 35 or those with high levels of Follicular stimulating hormone (FSH). Typically one may opt for this method after the failure of 2 or more IVF procedures. This procedure has also proven to be beneficial for women with poor embryo qualities.
Mini-IVF
Low AMH is one of the major causes of difficulty in conceiving. As a woman grows older, her AMH levels considerably reduce. If your AMH has reduced because of your age, increasing the hormone stimulation will not increase the number of eggs you produce. Mini-IVF is a process which is recommended for women who have low AMH because of their age.
Similar to the conventional IVF procedure, mini-IVF predominantly differs in terms of lesser usage of oral medications for hormonal stimulation. It is generally considered to be a milder and toned-down version of a conventional IVF procedure.
Younger women between the ages of 25-38 however, need not opt for this and they should first get tested to find the reason for their low AMH levels so that it can be cured. If their AMH can be clinically increased they’ll easily be able to conceive either naturally or IVF. Many women feel that they’ll have to compromise on their career and conceive early to avoid difficulties in conceiving that one might face after the age of 35.
It’s best to get your eggs freezed before marriage so that you’re not stressed about decrease in your AMH levels. This will give you psychological guilt freedom.
Gonadotropin-releasing hormone.
The Gonadotropin-releasing hormone or GnRH is a very important hormone that triggers the release of Follicular stimulating Hormone(FSH) and the Luteinizing Hormone (LHG) that aids fertility. With regards to GnRH there are two important specifications: GnRH agonist and GnRH antagonist. The primary difference between the two treatments is that the agonist creates an initial surge in levels of FSH and LH whereas the antagonist does not. These hormones play a vital role In ovarian stimulation and help improve IVF success rates.
While undergoing this treatment women must be cautious of the potential side effects it may bring including headaches, nausea, and even rashes. This treatment is particularly recommended for women suffering from endometriosis and studies have shown that the results are rather good. This treatment is a bit more on the long term spectrum as opposed to other treatments but is said to work well with a history of failed IVF attempts and women above the age of 35.
Each woman is different with different functioning of the body. Note that this article is meant to educate you about the latest techniques. Feel free to consult your doctor regarding any of these options.
About The Author
 Dr. Hrishikesh Pai, M.D, F.R.C.OG (UK), F.C.P.S, F.I.C.O.G, M.Sc (USA) is a pioneer in the field of IVF. Dr. Pai’s notable achievements include being awarded with the esteemed fellowship ad eundem of the Royal College of Obstetricians and Gynecologists, London, UK, Serving as the past president of ISAR, IAGE and MOGS and with over 30 awards in various fields for lifetime achievements. He is also the Director of the Bloom IVF Group.
Dr. Hrishikesh Pai, M.D, F.R.C.OG (UK), F.C.P.S, F.I.C.O.G, M.Sc (USA) is a pioneer in the field of IVF. Dr. Pai’s notable achievements include being awarded with the esteemed fellowship ad eundem of the Royal College of Obstetricians and Gynecologists, London, UK, Serving as the past president of ISAR, IAGE and MOGS and with over 30 awards in various fields for lifetime achievements. He is also the Director of the Bloom IVF Group.
Bloom IVF Group is India’s premier provider for fertility, IVF, and other assisted conception treatments with over 25,000+ patients from India and abroad. It is one of the largest groups of IVF centers in India with 10 full fledged IVF centers up to date with all the latest IVF techniques. Their main aim is to offer the latest services in the field with success rates equivalent to the western world, at very affordable costs, but without any compromise on quality.
For more information, contact at 9871717305 or email at contact@bloomivfgroup.com.
Prenatal sex determination and sex selection is illegal in India and not done here.





Your Comment Is Valuable For Us
Thanks For Your Feedback.